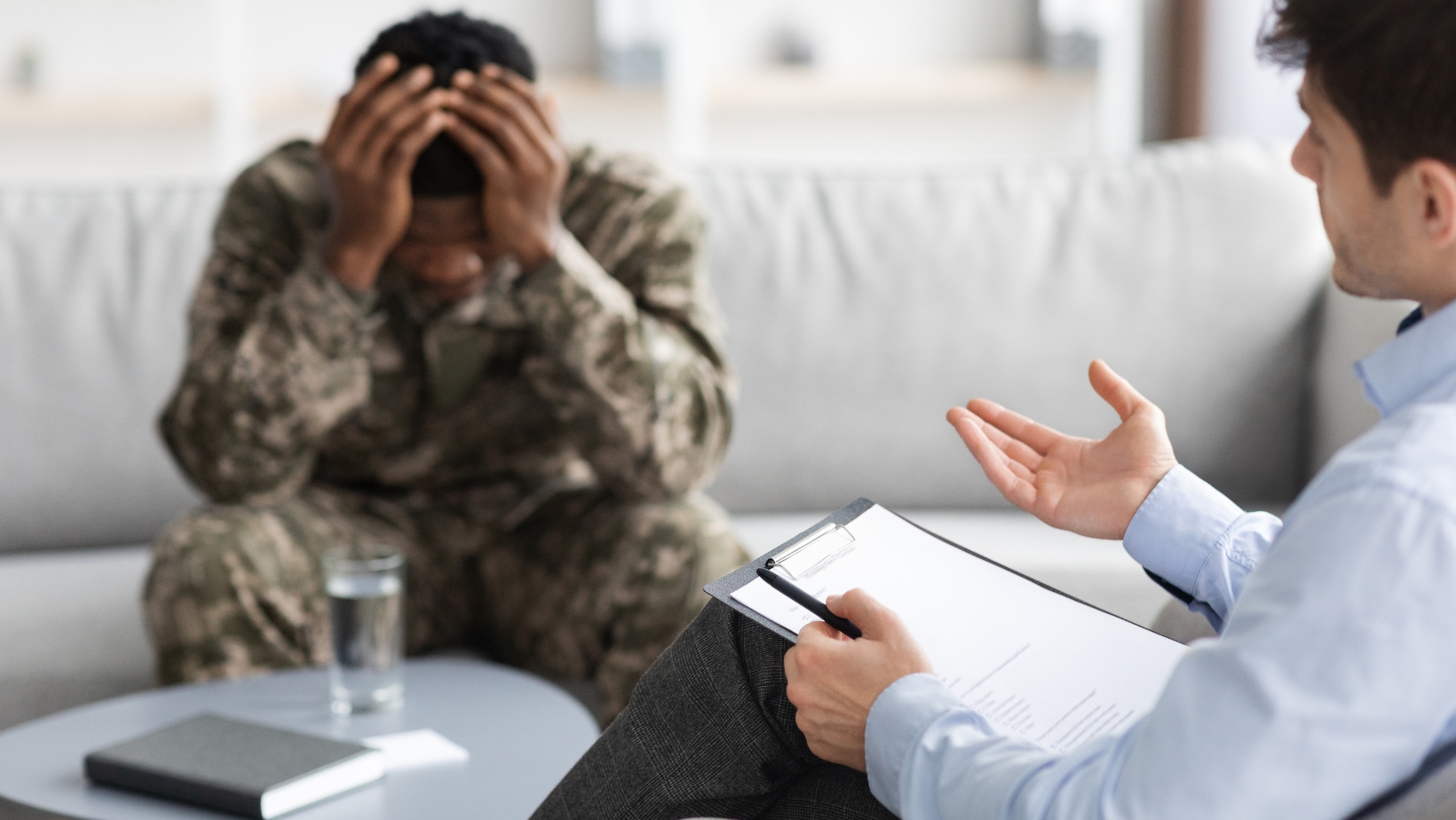
Post-Traumatic Stress Disorder (PTSD) affects millions of individuals worldwide, often leaving them feeling overwhelmed, misunderstood, and unsupported. For these individuals, accessing care that prioritizes safety, understanding, and empowerment is critical. Trauma-informed care (TIC) is an approach that recognizes the impact of trauma on mental health and tailors interventions to meet the unique needs of those affected.
In this article, we’ll explore the principles of trauma-informed care, how it supports PTSD patients, and why it’s essential for effective treatment and recovery.
Understanding Trauma-Informed Care
Trauma-informed care (TIC) is a framework used across healthcare, mental health, and social service settings to create an environment that acknowledges the prevalence and impact of trauma. It prioritizes compassion, safety, and empowerment, ensuring that patients feel respected and understood.
TIC is not a specific therapy or treatment; rather, it’s an approach that guides professionals in delivering care in a way that avoids retraumatization.
The Prevalence of Trauma and PTSD
Trauma is more common than many people realize, and its effects are far-reaching. According to the National Center for PTSD**, around 6% of adults in the U.S. will experience PTSD at some point in their lives. Factors such as childhood abuse, combat exposure, sexual assault, and natural disasters are common triggers.
Because trauma is so pervasive, many individuals seeking healthcare or mental health services may have a history of traumatic experiences, whether disclosed or not. This makes trauma-informed care an essential practice across all professional settings.
The Core Principles of Trauma-Informed Care
Trauma-informed care is built upon six guiding principles that emphasize safety, collaboration, and respect for the patient’s experiences.
1. Safety
Creating a physically and emotionally safe environment is the cornerstone of TIC. Patients should feel secure in their interactions with professionals and their surroundings.
Example:
Providing a calm, private space for therapy sessions or medical exams helps reduce anxiety for individuals with PTSD.
2. Trustworthiness and Transparency
Building trust through clear communication and consistent practices is vital. Patients should understand what to expect from their care and feel that their providers have their best interests at heart.
Example:
Explaining procedures step-by-step can ease a PTSD patient’s fears and help them feel more in control.
3. Peer Support
Connecting patients with peers who have similar experiences fosters a sense of community and validation.

Peer support groups provide an emotional understanding that complements professional care.
4. Collaboration and Mutuality
TIC emphasizes a partnership between providers and patients. Patients are seen as active participants in their recovery rather than passive recipients of care.
Example:
Including patients in decisions about their treatment plan empowers them to take ownership of their healing process.
5. Empowerment, Voice, and Choice
TIC recognizes the strengths and resilience of trauma survivors, ensuring that care supports their autonomy and respects their choices.
6. Cultural, Historical, and Gender Awareness
Care must be sensitive to cultural, racial, and gender dynamics that shape a patient’s experience of trauma. Providers are encouraged to adapt their practices to meet the unique needs of diverse populations.
How Trauma-Informed Care Supports PTSD Patients
Trauma-informed care helps PTSD patients by addressing the emotional, psychological, and physical effects of trauma in a compassionate and supportive manner.
1. Minimizing Retraumatization
For PTSD patients, certain environments or interactions can trigger flashbacks or anxiety. TIC minimizes these risks by creating a sense of safety and predictability.
Example:
A healthcare provider might allow a patient to bring a trusted friend or family member to appointments to help them feel more comfortable.
2. Fostering Emotional Safety
TIC creates an environment where patients feel heard and validated. This emotional safety is critical for patients to process trauma and engage in treatment.
Example:
Therapists trained in TIC avoid pressuring patients to share traumatic memories before they feel ready.
3. Promoting Recovery and Resilience
TIC helps patients recognize their own strengths and supports them in building skills to manage PTSD symptoms.
Example:
Therapists may use techniques like Cognitive Behavioral Therapy (CBT) or Eye Movement Desensitization and Reprocessing (EMDR) within a trauma-informed framework to address negative thought patterns and reprocess traumatic memories.
Examples of Trauma-Informed Practices
Healthcare Settings
– Training staff to recognize signs of trauma and respond sensitively.
– Adjusting medical procedures to accommodate patients with PTSD (e.g., allowing breaks during exams).
Mental Health Services
– Using grounding techniques to help patients manage distress during therapy sessions.
– Offering telehealth options for individuals who may feel unsafe leaving their homes.
Schools and Community Organizations
– Providing trauma-informed training for teachers to support students affected by trauma.
– Establishing community centers where survivors can access peer support and counseling.
Benefits of Trauma-Informed Care
Trauma-informed care provides significant benefits for both patients and professionals:
– Improved Patient Outcomes: Patients feel more engaged in their treatment and experience reduced symptoms of PTSD.
– Stronger Relationships: Trust between patients and providers fosters a sense of safety and collaboration.
– Enhanced Provider Effectiveness: Professionals trained in TIC are better equipped to manage challenging situations and avoid burnout.
Research Insight:
A study published in Psychological Trauma: Theory, Research, Practice, and Policy found that trauma-informed care reduced PTSD symptoms by 40% and improved patient satisfaction rates in clinical settings.
Challenges in Implementing Trauma-Informed Care
Despite its benefits, TIC is not without challenges:
1. Lack of Training: Many providers lack formal education in trauma-informed practices.
2. Systemic Barriers: Overburdened systems and limited resources can make it difficult to implement TIC effectively.
3. Cultural Competence: Ensuring care is sensitive to diverse experiences of trauma requires ongoing effort and awareness.
Moving Forward: The Future of Trauma-Informed Care
As awareness of trauma’s impact grows, the adoption of TIC is becoming more widespread across various fields. Continued research, training, and advocacy will ensure that more patients benefit from this compassionate approach to care.
Conclusion
Trauma-informed care is a transformative approach that recognizes the profound effects of trauma and seeks to provide support that is safe, empowering, and respectful. For PTSD patients, TIC offers a path to healing that acknowledges their experiences and prioritizes their well-being.
By embracing trauma-informed practices, professionals can make a meaningful difference in the lives of those affected by trauma, fostering recovery, resilience, and hope for the future.
